Urinary incontinence is the involuntary leakage of urine caused by changes in bladder control, pelvic floor muscle function, or nervous system signaling. It is more common in women than in men, particularly due to reproductive health events such as pregnancy, childbirth, and menopause. While it is common, it is not a normal part of aging—and most cases are highly treatable with the right care.
Despite affecting more than 25 million adults in the United States, more than 4 in 10 women aged 65 and older experience urinary incontinence. The risk increases with age, especially after 50. Urinary incontinence affects twice as many women as men, often due to reproductive health events unique to women. Chronic urinary incontinence is a persistent form of the disorder. Although it can occur at any age, it is more common in women over 50. Many people delay treatment due to embarrassment or the belief that nothing will help.
Introduction to Urinary Incontience
Urinary incontinence, or loss of bladder control, is a widespread condition that affects people of all ages and backgrounds. It occurs when the bladder muscles and pelvic floor muscles are unable to work together effectively, leading to involuntary urine leakage.
There are several types of urinary incontinence, each with distinct causes and symptoms, including stress incontinence, urge incontinence (overactive bladder), mixed incontinence, and overflow incontinence. While it can be distressing, understanding the underlying issues—such as weak pelvic floor muscles or changes in bladder control—can help guide effective treatment.
This article explores the different types of urinary incontinence, what causes them, how they are diagnosed, and the most effective ways to manage and improve bladder control.
How Urinary Incontinence Affects Daily Life
Urinary incontinence impacts far more than bladder function. The primary symptom is urine leakage before reaching the bathroom or during activities such as sneezing, coughing, laughing, or exercising.
Many people experience changes in:
- Exercise and physical activity
- Sleep quality
- Work and social confidence
- Sexual health and intimacy
Even mild leakage can create ongoing stress, which may further worsen bladder symptoms through increased pelvic floor muscle tension.
Functional incontinence can occur when physical limitations or disabilities prevent timely access to a restroom, leading to urine leakage.
Common Symptoms of Urinary Incontinence
Symptoms vary depending on the underlying cause and may include:
- Urine leakage with movement, coughing, or exercise
- Sudden urinary urgency followed by leakage
- Frequent urination or nighttime urination
- Difficulty holding urine
- Dribbling or incomplete bladder emptying
Keeping a bladder diary may help identify patterns in urination and can be used as part of bladder training to improve bladder control. Identifying symptom patterns helps guide effective treatment.
Types of Urinary Incontinence
Urinary incontinence is not a single condition. There are four main types: stress, urge, functional, and overflow incontinence. The two most common types affecting women are stress incontinence and urge incontinence, also known as overactive bladder.
Understanding the type is essential for choosing the right treatment approach. Many women experience a combination of stress and urge incontinence, referred to as mixed incontinence.
Stress Incontinence
Leakage occurs when pressure is placed on the bladder, such as during coughing, sneezing, or exercise.
Urge Incontinence (Overactive Bladder)
Urge incontinence is characterized by urinary urgency—a sudden, intense need to urinate—followed by involuntary leakage. This condition is often linked to bladder or pelvic floor muscle overactivity. Anticholinergic medications are commonly prescribed to treat overactive bladder and urge incontinence.
Mixed Urinary Incontinence
Many women experience both stress and urge symptoms, a condition known as mixed urinary incontinence. Treatment must address both muscle coordination and bladder signaling.
Overflow Urinary Incontinence
Leakage caused by incomplete bladder emptying is often related to pelvic floor tension, nerve issues, or prostate problems.
Causes and Risk Factors
Urinary incontinence can develop for many reasons, often involving a combination of physical, medical, and lifestyle factors. Weakness or dysfunction of the pelvic floor muscles is a leading cause, especially after pregnancy, vaginal birth, or pelvic surgery. Hormonal changes during menopause can also weaken the support structures of the urinary tract.
Certain medical conditions—such as benign prostatic hyperplasia (enlarged prostate), multiple sclerosis, diabetes, and chronic urinary retention—can disrupt nerve signaling between the bladder and brain. Prostate surgery in men and pelvic organ prolapse in women are additional risk factors.
Other contributors include chronic constipation, obesity, frequent heavy lifting, and persistent coughing, all of which place extra pressure on the bladder and pelvic organs. While aging is associated with changes in bladder muscle function and elasticity, urinary incontinence is not inevitable.
Lifestyle habits, including high intake of bladder irritants such as caffeine and alcohol, can worsen symptoms. A family history of urinary incontinence or connective tissue disorders may also increase susceptibility. Understanding these risk factors is essential for creating a personalized treatment plan.
Pelvic Floor
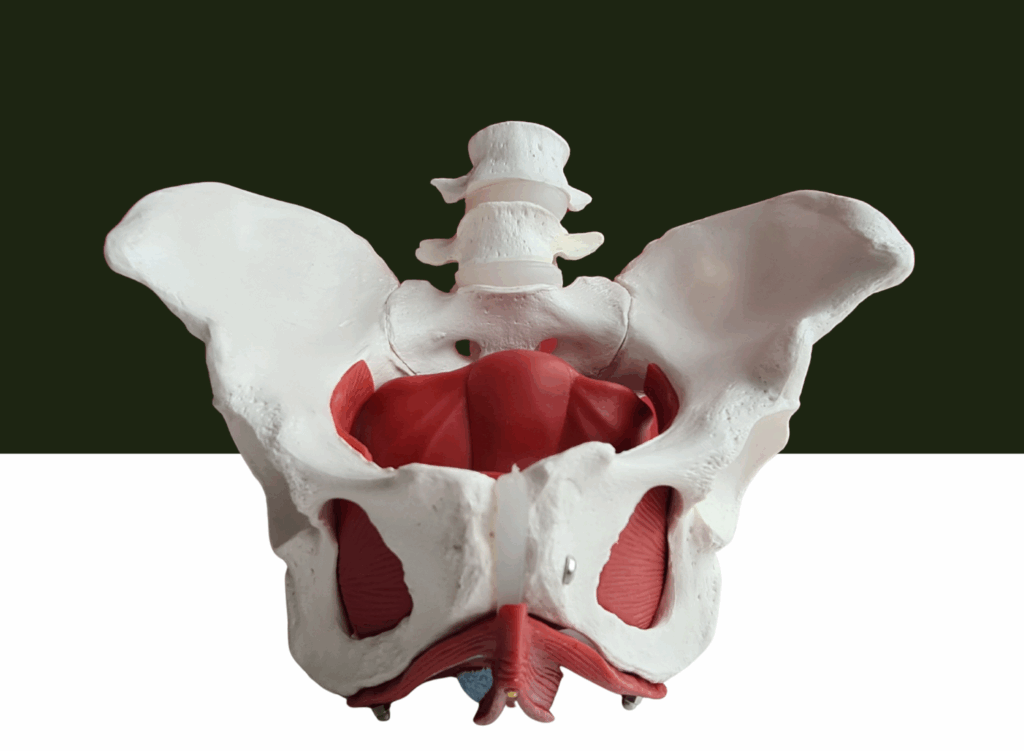
The pelvic floor is a group of muscles that support the bladder, bowel, and reproductive organs.
Pelvic floor muscles may be weakened by pregnancy, childbirth, aging, hormonal changes during menopause, and certain neurological conditions. These muscles play a critical role in maintaining bladder control. Pelvic floor muscle training—such as Kegel exercises—is important for preventing urinary incontinence and supporting pelvic organ health.
Healthy pelvic floor muscles must:
- Contract when needed
- Relax fully
- Coordinate with breathing and movement
When this balance is disrupted, bladder control suffers.
Female Urinary System
The female urinary system is especially vulnerable due to:
- Pregnancy-related muscle strain
- Hormonal changes during menopause
- Changes in pelvic organ support
Pregnancy increases pressure on the bladder and pelvic floor muscles, while childbirth—particularly vaginal delivery—can weaken muscles and damage nerves that control bladder function. Hormonal shifts during menopause can weaken the urethra and bladder neck, increasing the risk of urinary incontinence.
Although these factors raise risk, targeted therapy can restore function.
Treatment Options That Actually Work
Urinary incontinence is a common condition that can significantly impact quality of life, but it is highly treatable. Treatment options depend on the type and severity of symptoms and may include behavioral therapies, medications, nerve stimulation, and surgery.
Pelvic Floor Exercises

Pelvic floor exercises are a cornerstone of treatment—but only when performed correctly.
A pelvic floor therapist can help:
- Determine whether muscles are weak or overactive
- Teach proper muscle coordination
- Prevent worsening symptoms
Generic exercises without professional assessment often fail.
Kegel Exercises
Kegel exercises can strengthen pelvic floor muscles, but they are not appropriate for everyone. If the muscles are already tight or overactive, Kegels may worsen urgency and leakage. Professional guidance ensures the correct approach.
Prevent Urinary Incontinence
You can help prevent urinary incontinence by:
- Addressing pelvic floor dysfunction early
- Avoiding chronic straining
- Managing constipation
- Reducing bladder irritants such as caffeine and alcohol
- Practicing proper breathing and posture
Prevention focuses on function—not just strength.
Advanced Therapies for Persistent Symptoms
When conservative treatments are not effective, advanced options may be considered. Surgical treatments include sling procedures, bladder suspension, and artificial urinary sphincters. The artificial urinary sphincter is primarily used for men with severe urinary incontinence.
Another minimally invasive option is urethral bulking agents, which are injected around the urethra to improve closure and prevent leakage. These therapies are typically reserved for persistent cases.
Nerve Stimulation
Nerve stimulation therapies help regulate bladder signaling and reduce urinary urgency. They are especially helpful for overactive bladder and mixed incontinence.
Percutaneous Tibial Nerve Stimulation (PTNS)
PTNS is a minimally invasive therapy that:
- Modulates bladder nerve pathways
- Reduces urgency and frequency
- Improves bladder control
It is supported by clinical research and is often combined with pelvic floor therapy.
Why Pelvic Floor Physical Therapy Is First-Line Care
According to the American Physical Therapy Association (APTA), pelvic floor physical therapy is a recommended first-line treatment for urinary incontinence.
Therapy may include:
- Muscle retraining
- Manual therapy
- Bladder retraining
- Breathing coordination
- Nervous system regulation
Why Choose Pelvis NYC?
Pelvis NYC specializes in pelvic floor physical therapy and treats urinary incontinence across all genders and life stages.
Patients benefit from:
- One-on-one expert care
- Evidence-based treatment
- Trauma-informed, judgment-free sessions
👉 Book a consultation with Pelvis NYC to treat urinary incontinence at its root—not just manage symptoms.
Frequently Asked Questions (FAQ)
What causes urinary incontience?
Urinary incontinence can result from pelvic floor dysfunction, bladder issues, nerve signaling problems, hormonal changes, or prostate conditions. The urethral sphincter plays a critical role in maintaining continence by keeping the urethra closed during increases in abdominal pressure.
Is urinary incontinence normal with age?
It is common, but not normal or inevitable. Treatment is often highly effective.
Do Kegels help urinary incontinence?
Sometimes. If pelvic floor muscles are tight, relaxation may be needed before strengthening.
Can pelvic floor physical therapy cure incontinence?
Many people experience significant improvement or complete resolution with proper therapy.
When should I seek help?
If symptoms affect daily life, sleep, or confidence, seek care early.
How is urinary incontience diagnosed?
Diagnosis involves a thorough medical history, physical examination, and tests such as urinalysis and bladder diaries.
Where can I find reliable patient resources?
The American Urological Association and the National Association for Continence provide trustworthy patient resources.
Are digestive and kidney diseases related to urinary incontinence?
Yes. Digestive and kidney diseases can be associated with urinary incontinence. Organizations such as the National Institute of Diabetes and Digestive and Kidney Diseases focus on these conditions and their management.
Conclusion
Urinary incontinence is a common and treatable condition that can significantly affect daily life, but it does not need to be endured in silence. With accurate diagnosis and a personalized treatment plan—including pelvic floor therapy, lifestyle modifications, and advanced therapies—most people can regain bladder control and reduce or eliminate leakage.
Early intervention is key. If you or a loved one is experiencing symptoms, effective solutions are available to help treat urinary incontinence and restore confidence.