Hello there! If you’re navigating the world of lower abdominal pain, you’ve probably stumbled upon the question: “How can Physical Therapy help?” Lucky for you, I’m here to shed some light on the pivotal role Physical Therapy plays in easing lower abdominal pain. As a Physical Therapist, I’ve got the insider scoop on why it’s a game-changer.
Demystifying Lower Abdominal Pain
Before we dive into the magic of Physical Therapy, let’s demystify what’s going on in your lower abdominal region. It’s like peeling back the layers of an onion—we need to understand the root cause to effectively address the issue.
The Physical Therapy Plays for Easing Lower Abdominal Pain
1. Assessment Magic
Imagine your lower abdomen is a puzzle, and Physical Therapists are the puzzle masters. Through a thorough assessment, we pinpoint the exact areas causing you grief. It’s like having a GPS for your pain.
2. Tailored Treatment Plans
No one-size-fits-all nonsense here. Physical Therapy crafts personalized plans to suit your specific needs. It’s like having a custom-made suit for your lower abs—stylish and comfortable.
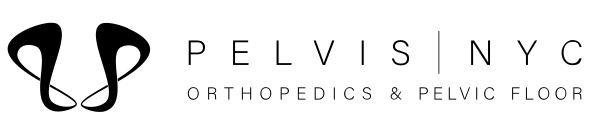
3. Hands-On Healing
Physical Therapists are like the wizards of touch. Through hands-on techniques, we work to alleviate tension and promote healing. It’s like a spa day for your lower abs, minus the cucumber slices.
4. Empowering Exercises
We don’t just do the work for you; we empower you with exercises that can help ease lower abdominal pain to continue the healing process at home. It’s like having a coach for your abs, cheering you on from the sidelines.
5. Educational Insights
Knowledge is power. We provide insights into lifestyle changes and habits that can contribute to long-term relief. It’s like having a roadmap to a pain-free life.
Wrapping It Up
There you have it! A glimpse into the powerful world of Physical Therapy and its crucial role in easing lower abdominal pain. Remember, I’m your virtual PT, here to guide you on your journey to relief.
If that lower abdominal pain is playing hard to get, don’t hesitate to reach out to Pelvis NYC. We are looking forward to a pain-free and empowered you!
Related Blog: Experts to Consult for Lower Left Abdominal Pain in Men