If you’re reading this, chances are you or someone you care about is dealing with Hard Flaccid Syndrome (HFS). Let me tell you, I know firsthand how frustrating and embarrassing this condition can be. The good news is that there are hard flaccid syndrome treatment options available that can help alleviate the symptoms.
Note: The first part of this blog story is written from the POV of one of our patients.
Introduction
When I first experienced Hard Flaccid Syndrome (HFS), I had no idea what was happening to my body. It seemed like nobody else was talking about this condition, and I didn’t know where to turn for help. I felt alone, confused, and embarrassed. However, through my research and conversations with our men’s group, I discovered a hard flaccid doctor who provides an effective hard flaccid syndrome treatment.
Whether you’re a man experiencing HFS or a partner looking to support someone who is, I want to provide you with the information and tools that were given to me by Dr. Adam Gvili– Doctor of Physical Therapy of Pelvis NYC. These help me find relief and reclaim my sexual health.
Hard Flaccid Syndrome Treatment Process
Before we start, I want to clarify that this treatment process was tailored to my needs by Dr. Gvili. Every treatment is different for every patient experiencing HFS. This is only a guide or preview of how physical therapy helps me regain my sexual potency.
- Assessment
The first step that was given to me by Dr. Adam was to undergo an assessment. During this process, he examined my pelvic area and conducted a thorough interview to gather information about my medical history and symptoms.
- Muscle strengthening
Since hard flaccid syndrome is caused by weakened pelvic floor muscles, he created a specific treatment plan for me. Dr. Gvili developed a personalized exercise plan to strengthen pelvic floor muscles and improve their function.
- Stretching
Tight or shortened muscles can also contribute to Hard Flaccid Syndrome. He also provides targeted stretches to help lengthen my muscles and reduce tension.
- Pain Management
Aside from the common treatment process prescribed by him, he also helped me manage my pain through various techniques such as massage, heat therapy, and manual therapy. These are so refreshing!
- Lifestyle modifications
Lifestyle habits can also contribute to the development of Hard Flaccid Syndrome. According to Dr. Adam, making lifestyle changes may be necessary to manage this condition effectively. He guided me on diet, hydration, and other lifestyle factors that impact pelvic floor function.
Pelvis NYC for Hard Flaccid Syndrome Treatment

Dr. Adam Gvili can work with patients to identify underlying causes contributing to their symptoms. He is also knowledgeable in guiding how to make changes that can improve pelvic floor function.
Also, Dr. Adam Gvili uses a holistic approach to hard flaccid syndrome treatment by developing a comprehensive plan for managing their symptoms and improving their overall quality of life.
Schedule your appointment today!
Now, let’s get deeper into what Hard flaccid syndrome is and the treatments.
Hard Flaccid Syndrome Treatment
Hard flaccid syndrome treatment focuses on reducing pelvic floor muscle tension, calming the nervous system, and restoring normal blood flow and sensation. The most effective approach is typically pelvic floor–focused physical therapy combined with targeted pain management and lifestyle adjustments. While symptoms can feel persistent, many people improve significantly with the right care.
Hard Flaccid Syndrome
Hard flaccid syndrome (HFS) is a functional pelvic health condition where the penis feels semi-rigid or tense while flaccid and is often accompanied by pain, numbness, or changes in erectile quality.
Although not yet formally classified in major diagnostic manuals, HFS is increasingly recognized by:
- Pelvic floor physical therapists
- Urologists
- Sexual medicine specialists
Clinically, hard flaccid is best understood as a neuromuscular and pelvic floor regulation issue, not a structural or permanent penile disorder.
Common Symptoms
People with hard flaccid syndrome commonly report:
- Semi-rigid or “hard” flaccid penis
- Reduced penile sensitivity or numbness
- Pelvic, perineal, or penile pain
- Erectile difficulties or weaker erections
- Cold, tight, or disconnected sensation
- Anxiety related to sexual performance
Symptoms often begin after periods of:
- Chronic stress or anxiety
- Excessive pelvic muscle tension
- Intense exercise or heavy lifting
- Prolonged sitting
- Sexual overuse or edging
These patterns help guide effective treatment strategies.
Pelvic Floor
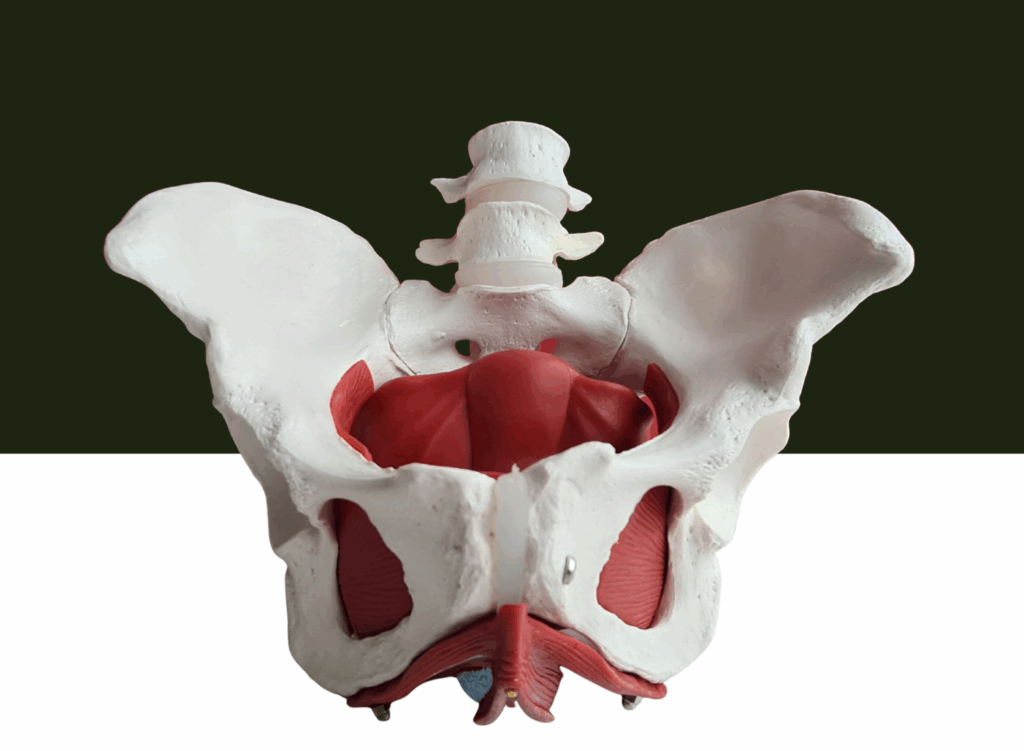
The pelvic floor is a group of muscles and connective tissues that support pelvic organs and play a key role in sexual function, urination, and circulation.
In hard flaccid syndrome, the pelvic floor often becomes:
- Chronically overactive
- Unable to fully relax
- Poorly coordinated with breathing and movement
This constant tension can compress nerves and restrict blood flow, contributing directly to symptoms.
Pelvic Floor Muscles
The pelvic floor muscles must be able to both contract and relax.
In many people with hard flaccid:
- Muscles remain stuck in a protective, contracted state
- Attempts to strengthen them (e.g., Kegels) increase tension
- Blood flow and nerve signaling are disrupted
This is why treatment focuses first on down-training and relaxation, not strengthening.
Pelvic Pain
Hard flaccid frequently overlaps with pelvic pain, including chronic pelvic pain syndromes in men.
Pelvic pain may present as:
- Aching or burning sensations
- Pressure in the perineum
- Discomfort during or after sexual activity
- Pain that worsens with sitting or stress
Research published in The Journal of Urology shows that pelvic pain conditions often improve when pelvic floor muscle dysfunction is addressed through targeted therapy rather than medication alone.
Pelvic Floor Physical Therapy

Pelvic floor physical therapy is widely considered the cornerstone of hard flaccid syndrome treatment.
This specialized therapy focuses on:
- Reducing excessive muscle tone
- Improving coordination and relaxation
- Normalizing nerve sensitivity
- Restoring healthy blood flow
A trained pelvic floor therapist evaluates muscle tone, breathing patterns, posture, and movement habits that may be perpetuating symptoms.
Physical Therapy
Unlike general physical therapy, physical therapy for hard flaccid requires specific training in male pelvic health.
Treatment may include:
- Manual therapy to release pelvic tension
- Breathing retraining
- Postural correction
- Nervous system regulation techniques
- Gradual return to normal activity
This whole-body approach is critical because pelvic floor dysfunction rarely exists in isolation.
Pelvic Floor Therapy
Pelvic floor therapy is not about quick fixes—it’s about retraining the system.
Most patients benefit from:
- Consistent sessions over several weeks or months
- Education to reduce fear-based muscle guarding
- Home exercises focused on relaxation and coordination
Clinical experience shows that patients who understand why symptoms occur tend to recover more effectively.
Pain Management

Effective pain management for hard flaccid addresses the source of pain rather than masking symptoms.
Common strategies include:
- Manual pelvic floor techniques
- Nervous system down-regulation
- Heat therapy or gentle movement
- Temporary activity modification
Medications may be helpful in some cases, but long-term improvement usually requires active rehabilitation.
Flaccid Syndrome
The term flaccid syndrome reflects the paradoxical nature of the condition—the penis appears flaccid but feels tense.
This paradox is explained by:
- Persistent muscle contraction
- Altered sensory feedback
- Dysregulated nervous system signaling
Understanding this mechanism helps patients move away from fear and toward recovery.
Hard Flaccid
So what does effective hard flaccid treatment actually look like in practice?
Successful treatment plans are typically:
- Individualized
- Focused on relaxation before strengthening
- Integrated with stress and lifestyle management
Many patients report gradual but meaningful improvements in comfort, sensation, and erectile quality.
Case Report
Although large-scale studies are limited, case reports and clinical observations provide valuable insight.
A commonly reported pattern includes:
- Initial worsening with strengthening exercises
- Symptom improvement after pelvic floor down-training
- Gradual normalization of flaccid state and erections
These findings align with broader research on male pelvic pain and pelvic floor dysfunction.
What Makes Treatment More Effective?
Based on clinical experience and emerging research, outcomes improve when patients:
- Seek care from pelvic floor specialists
- Avoid excessive strengthening early on
- Address stress and nervous system factors
- Stay consistent with therapy
Recovery timelines vary, but improvement is common when the underlying dysfunction is properly treated.
Frequently Asked Questions (Schema-Ready)
What is the best treatment for hard flaccid syndrome?
Pelvic floor physical therapy focused on muscle relaxation and nervous system regulation is considered the most effective treatment.
Can hard flaccid syndrome go away on its own?
Some mild cases improve, but many require targeted treatment to fully resolve.
Are Kegels good for hard flaccid?
In most cases, no. Strengthening exercises often worsen symptoms when muscles are already overactive.
How long does hard flaccid treatment take?
Many people see improvement within weeks to months, depending on severity and consistency of care.
Is hard flaccid syndrome permanent?
It is not considered permanent in most cases and often improves with proper treatment.
Final Takeaway
Hard flaccid syndrome treatment works best when it targets pelvic floor muscle tension, nervous system dysregulation, and pain—not just symptoms. With the right approach, many people experience meaningful improvement and regain confidence in their sexual and pelvic health.